Request Your Appointment
With our Dentist Near You
Richmond Dental Clinic Your Dentist in SW Calgary
If you are looking for a dentist in SW Calgary, AB, T3E 7C4, look no further than Richmond Dental Clinic. your trusted destination for comprehensive dental care in the Calgary area. Our team of experienced and caring professionals is dedicated to providing high-quality dental services to enhance oral health and create beautiful smiles.
We offer dental care services ranging from cosmetic tooth-whitening to simple essentials such as teeth-cleaning and maintenance to full restorative dentistry using implants, overdentures, crowns and bridges, veneers, and lumineers. Our dentist near you offers orthodontic treatment for adults and children and fits patients with sports, snore, and night mouthguards.
In addition to our regular services, our emergency dentistry is available when you call us, addressing your urgent dental needs promptly. Don’t hesitate to prioritize your oral health. Schedule an appointment today and let Richmond Dental Clinic be your partner in achieving a healthy and beautiful smile.
Advance Technology
Our dentist near you uses the latest and greatest dental technology to ensure the comfort of our patients.
Friendly Team
Our SW Calgary dentists are caring and compassionate. Come by our office and see the difference!
One-Stop Services
There’s no need to travel around Calgary to get the treatment you need. Visit Richmond Dental today.
Our Services
Laser Gum Surgery
If you are in need of periodontal surgery, then you have a choice between traditional treatment and laser treatment.
Invisalign
If you have misaligned teeth, you may have been putting off orthodontic treatment for one reason or another.
Dental Implants
If you are losing your teeth or have already lost one or more teeth, dental implants can replace your missing teeth
Root Canal
The dental pulp is located in the center of the tooth, underneath the layers of enamel and dentin.
Our SW Calgary Dental Clinic Gallery
Restoring your Oral Health

Facial Cosmetics
Did you know? Those pesky fine lines, wrinkles, and hollow cheeks can all be traced back to one source: reduction in facial volume. Unfortunately, as we age loss of skin elasticity and reduced collagen production take a toll on our bodies, but what can be done? Richmond Dental in Calgary is here to tell you that, thanks to neuromodulator Injections, firm, youthful skin is possible at any stage of life. Let’s talk about facial cosmetics with a dentist in SW Calgary and what they do for you.
Neuromodulator Injections are substances approved by the FDA to be injected under the skin to produce a smoother, firmer result. Contrary to popular belief, neuromodulator Injections can be used for much more than just filling in wrinkles. They can also be used to:

Teeth Whitening
Have you ever wondered why you have dull, stained or even discolored teeth but none of the stars in the movies or shows do? The answer is pretty simple, professional teeth whitening! At Richmond Dental we are proud to offer teeth whitening in SW Calgary for our patients that are interested in achieving a more healthy-looking, white and bright smile. Interested in scheduling your Calgary professional teeth whitening appointment? Contact Richmond Dental today; we’d be happy to get you added to our schedule for an appointment.
Have you ever tried over-the-counter teeth whitening treatments only to be left with sensitive teeth, damaged gums and no difference in the color of your smile? When it comes to store-bought teeth whitening treatments, they are often designed only to remove exterior staining (which your toothbrush could remove, leaving interior staining and a dull looking smile. With professional teeth whitening in Calgary, our whitening products are designed to achieve results fast, without the discomfort, sensitivity or damage to the tooth or gums.

Invisalign
These aligners are worn for a period of 20-22 hours per day and gently shift any teeth that need to be corrected into place. Although some patients find the process a little uncomfortable at first, they are still considered to be far more comfortable than traditional metal braces. But along with the increased comfort of Invisalign®️ aligners over other options, they have another huge advantage in that they can be taken out for special occasions. Important date coming up? You can remove your aligners! Important job interview coming up? You can remove your aligners! That’s how these remain a secret to only you and your dentist in Calgary! For Invisalign®️ Braces in SW, Calgary get in touch with the dentists at Richmond Dental today and avail the unparalleled services.
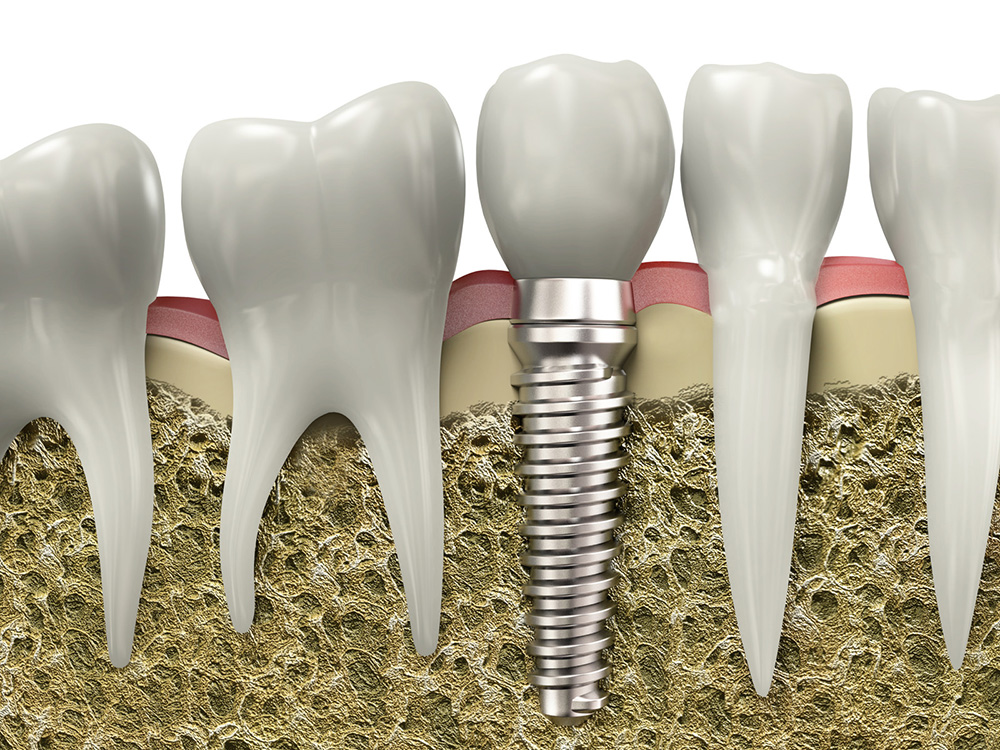
Dental Implants
The procedure known as a dental implant was developed to provide a structural foundation that replacement teeth can adhere to in a manner that looks and functions just like the natural teeth they are replacing. One of the biggest benefits of a dental implant near you is that they help patients maintain the quality of their jawbone. Additionally, since missing teeth can create alignment concerns for a patient’s remaining teeth, implants are used to fill the gap. This helps maintain oral health over a longer period of time.
At Richmond Dental our dental experts provide the best services concerning dental implants in SW, Calgary using the latest state-of-art technology equipments and techniques.

Why Choose Us?
Our practice offers dental care services ranging from cosmetic tooth-whitening to simple essentials such as teeth-cleaning and maintenance to full restorative dentistry using implants, overdentures, crowns and bridges, veneers, and lumineers. Our dentist in Calgary offers orthodontic treatment for adults, as well as children, and fit patients with sports, snore, and night mouthguards.
Further, we are skilled in performing root canals, removal of wisdom teeth, and the use of TMJ splints. For your comfort, we offer sedation dentistry as well. Our emergency dentistry is available on the day that you call us. Our dentist can truly serve all your dentistry needs.